IVF laboratory billing is where prospective invoices created by the embryology team will live until they are converted by the billing team to work as a new invoice.
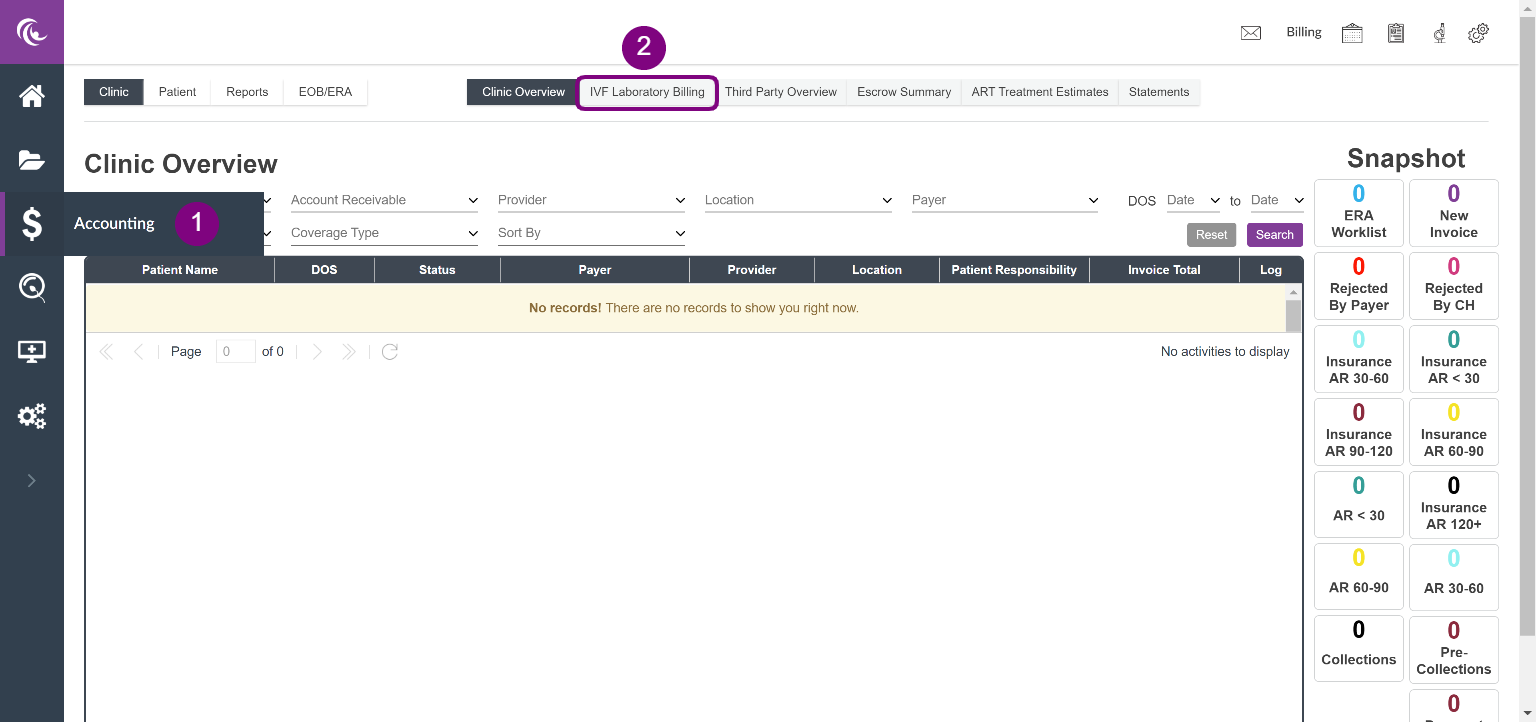
Navigation
- To navigate to IVF Laboratory Billing, click on Accounting in your navigational tools.
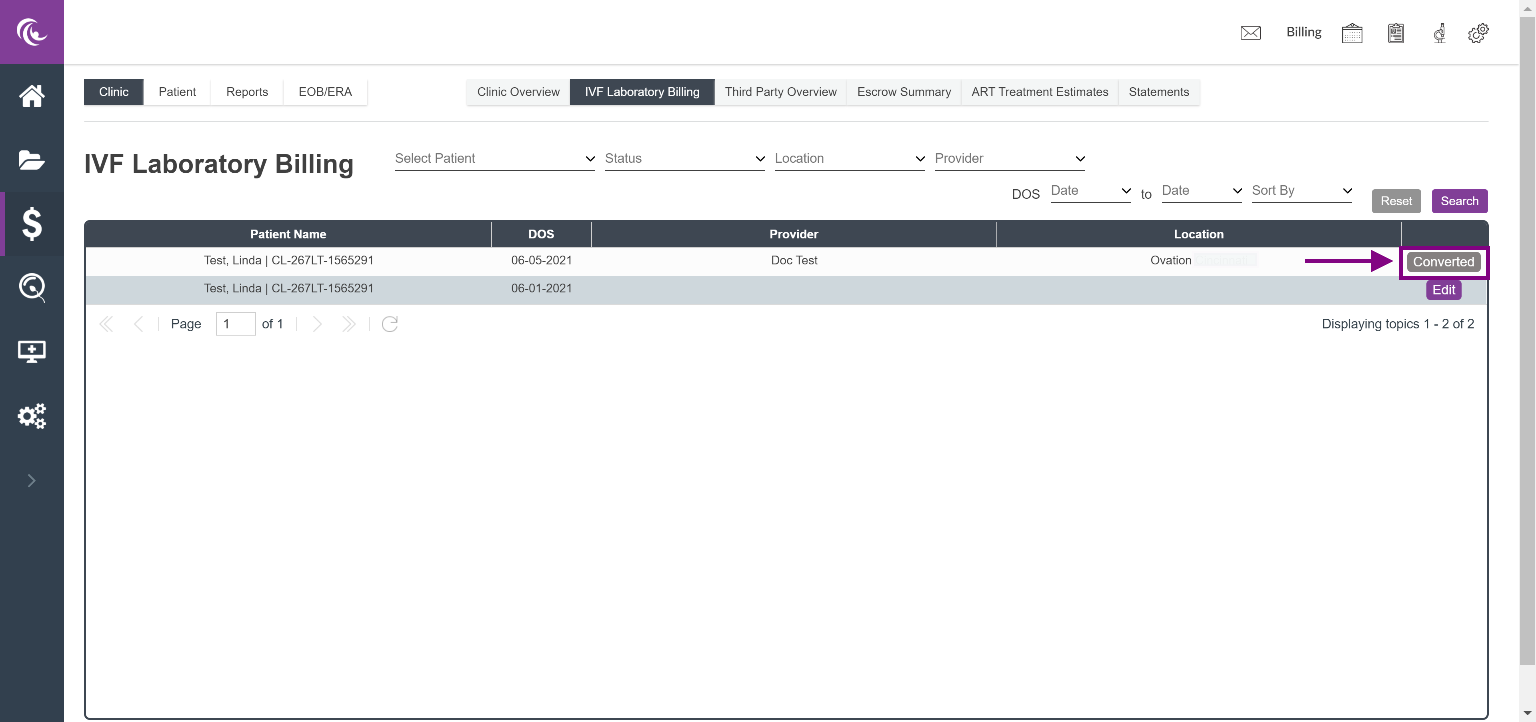
- In the Clinic Overview screen, click on the IVF Laboratory Billing tab in the top center of your screen.
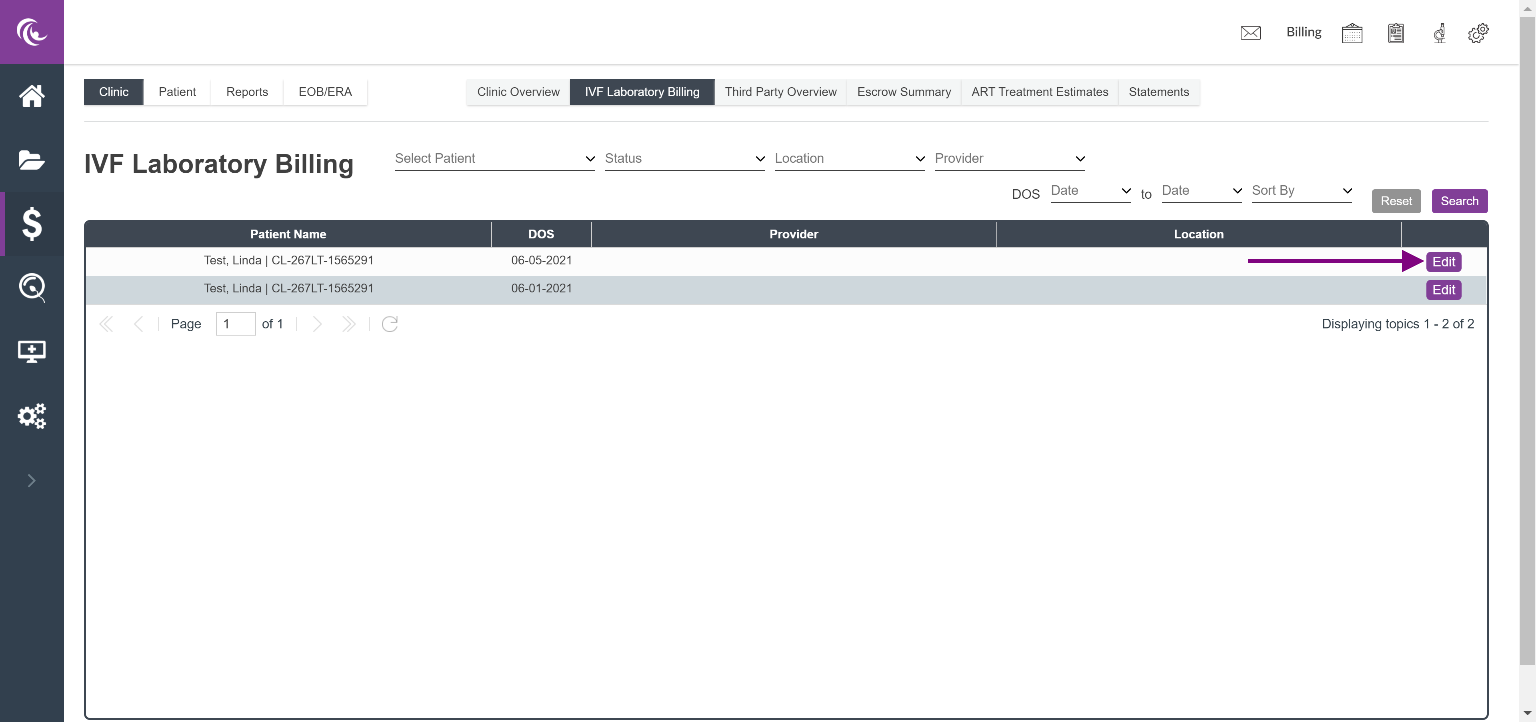
The IVF laboratory billing screen will display patients who had prospective invoices created by the embryology team. To edit an invoice, click Edit.
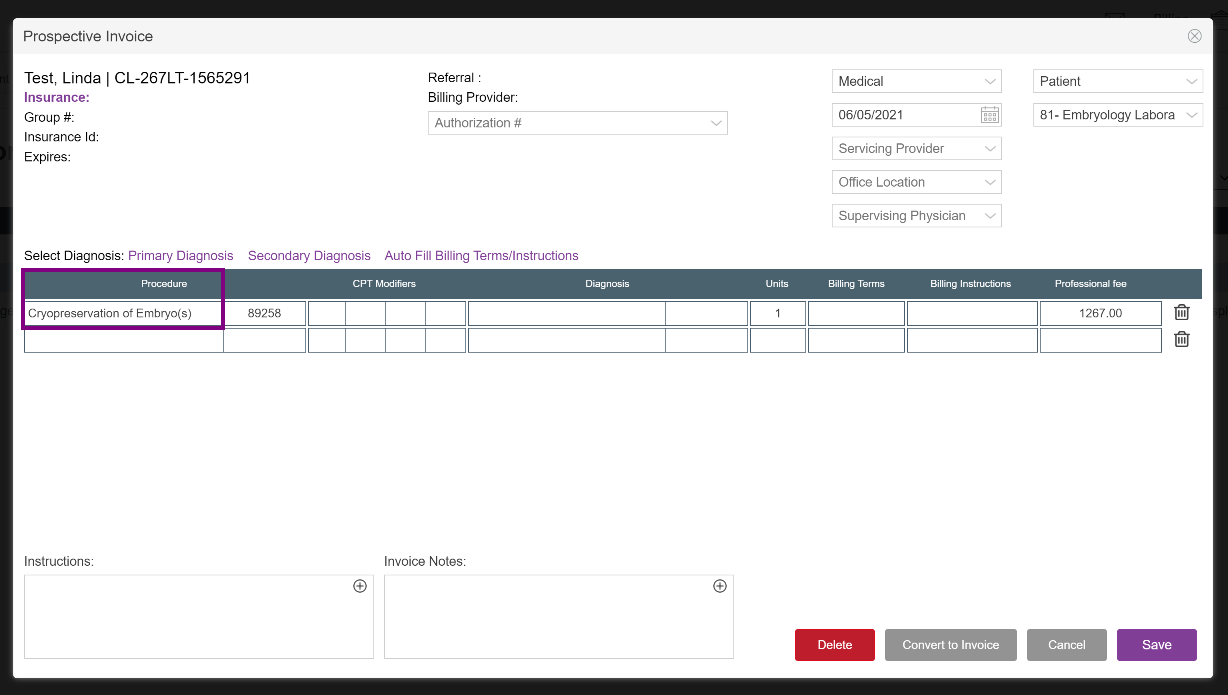
Completing a Prospective Invoice
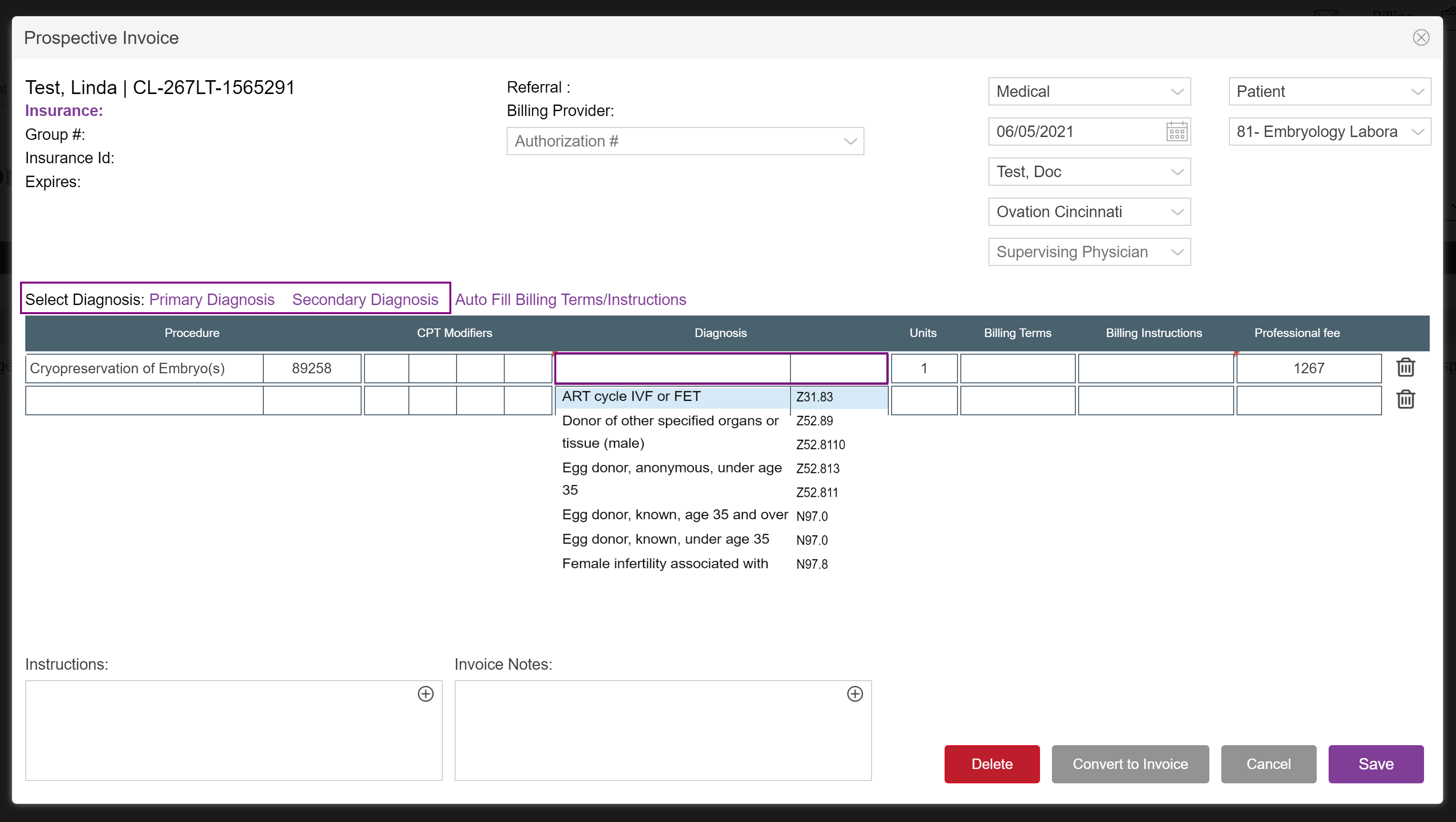
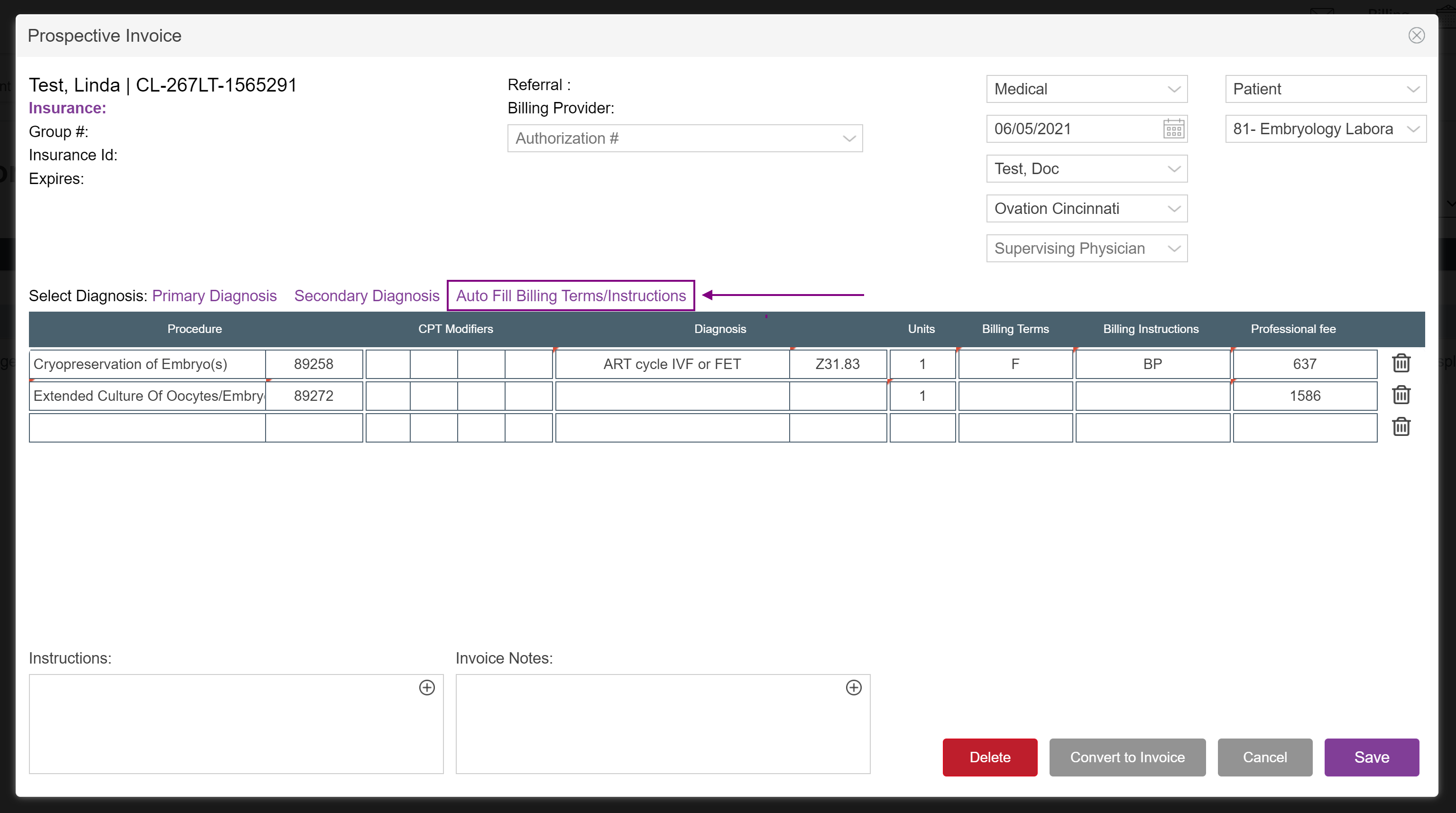
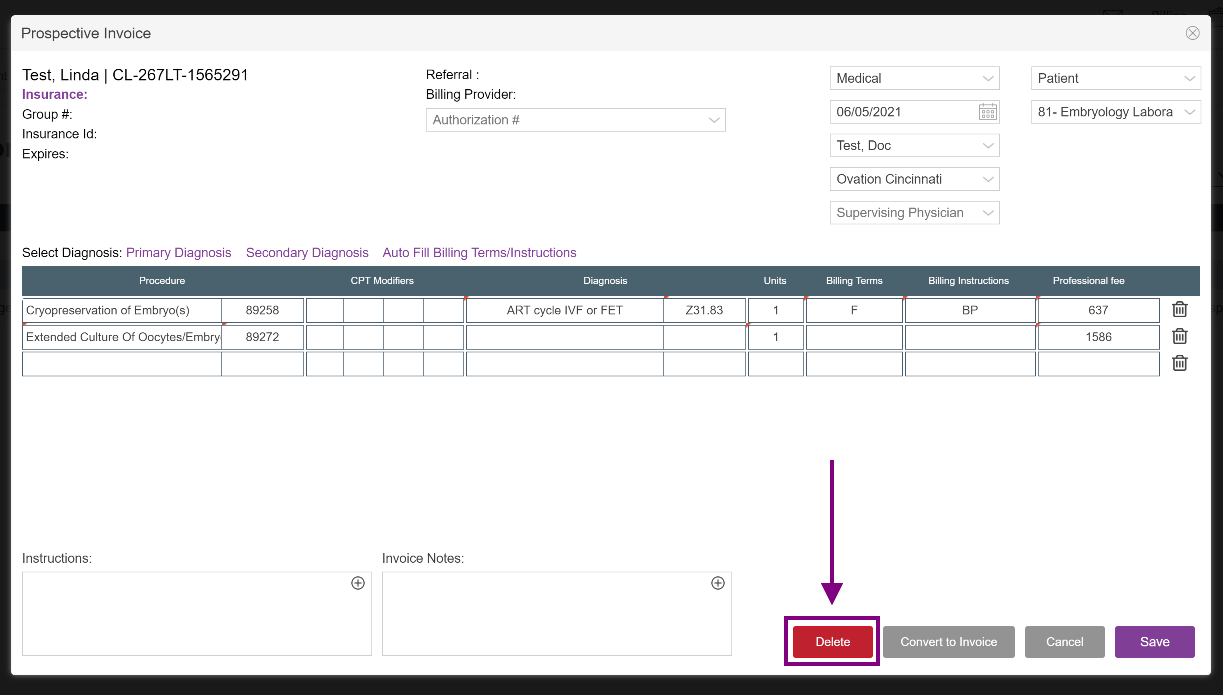
The Prospective Invoice screen will open and display the Procedures/CPT codes already associated with this specific appointment type. To learn more about managing CPT codes associated with appointment types, click here
The following items can be adjusted on the prospective invoice:
- Claim type - Medical or Surgical (defaults to Medical)
- Date of Service
- Provider
- Location
- Invoice for - patient or partner (defaults to Patient)
- Place of Service type (defaults to 81 - Embryology Laboratory)
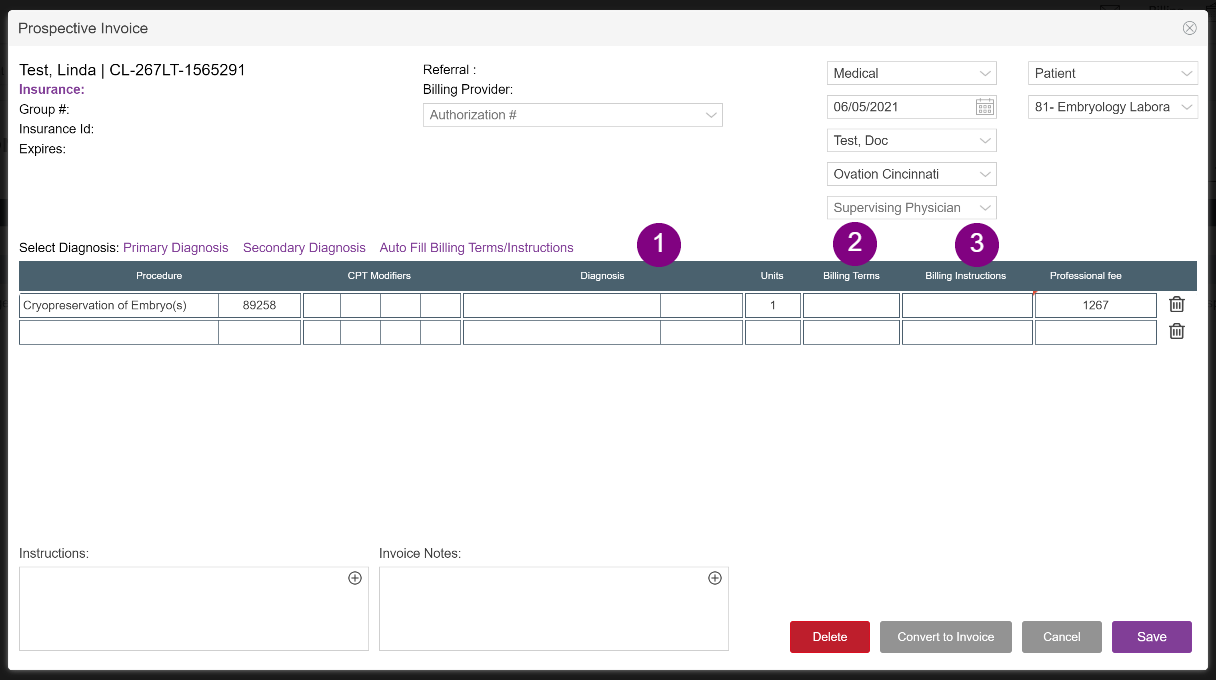
Enter the following for each line item:
- Diagnosis by description or ICD-10 code
- Billing Terms: Fee for Service (F), Package Plan (Pkg), or No Charge (N/C)
- Billing Instructions: Use the drop down menu to select if this will be billed to Patient, Insurance, etc.
Selecting Diagnoses
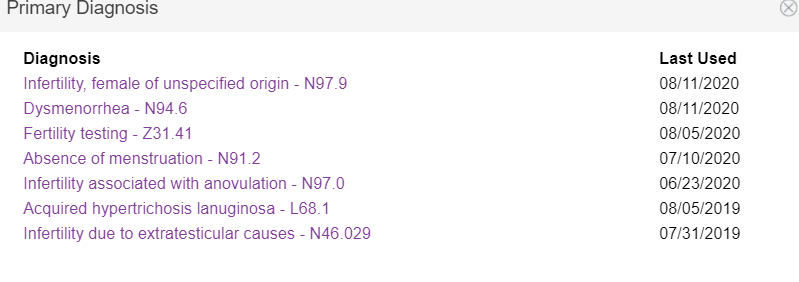
You may select the Diagnosis from previous diagnoses that have been assigned in the Primary/Secondary Diagnosis hyperlinks or from the pull down lists by description or ICD-10 codes. If you wish to add new secondary diagnoses, head over to our article to learn more about How to Enter Multiple ICD Codes.
When clicking on the hyperlink it will pull up all previous diagnoses used and the date of the last used. Click on the name of the one for this invoice to auto-populate to all line items.
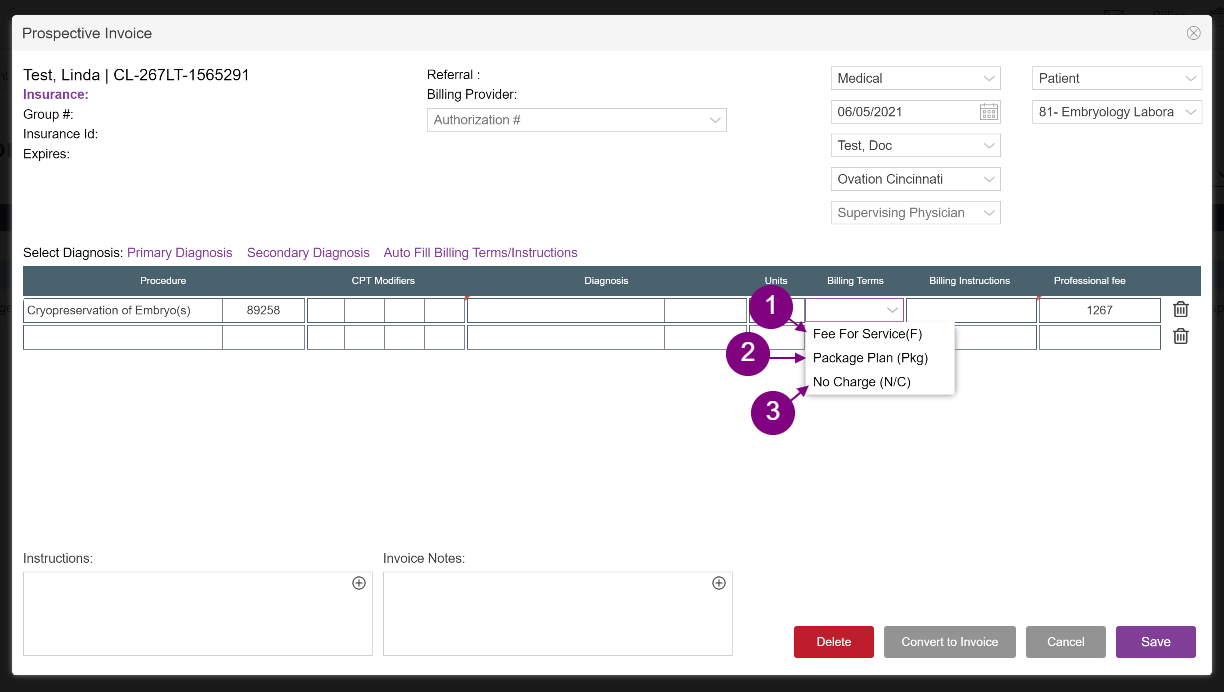
Billing Terms
Terms selected will label and determine the actions against the charges of the service line. Users may select from three options:
- Fee for Service (F) - this is the office's standard fee for that CPT code.
- Package Plan (Pkg) - selecting this term will associate the line item with a package plan recorded in the patient's escrow of their financial chart. Based on how the package plan is set up, the charges will either zero out or move money over from that package plan to satisfy the balance.
- No charge (N/C) - this term will automatically zero out the charges of the service line; if selected, billing instructions are not necessary to select.
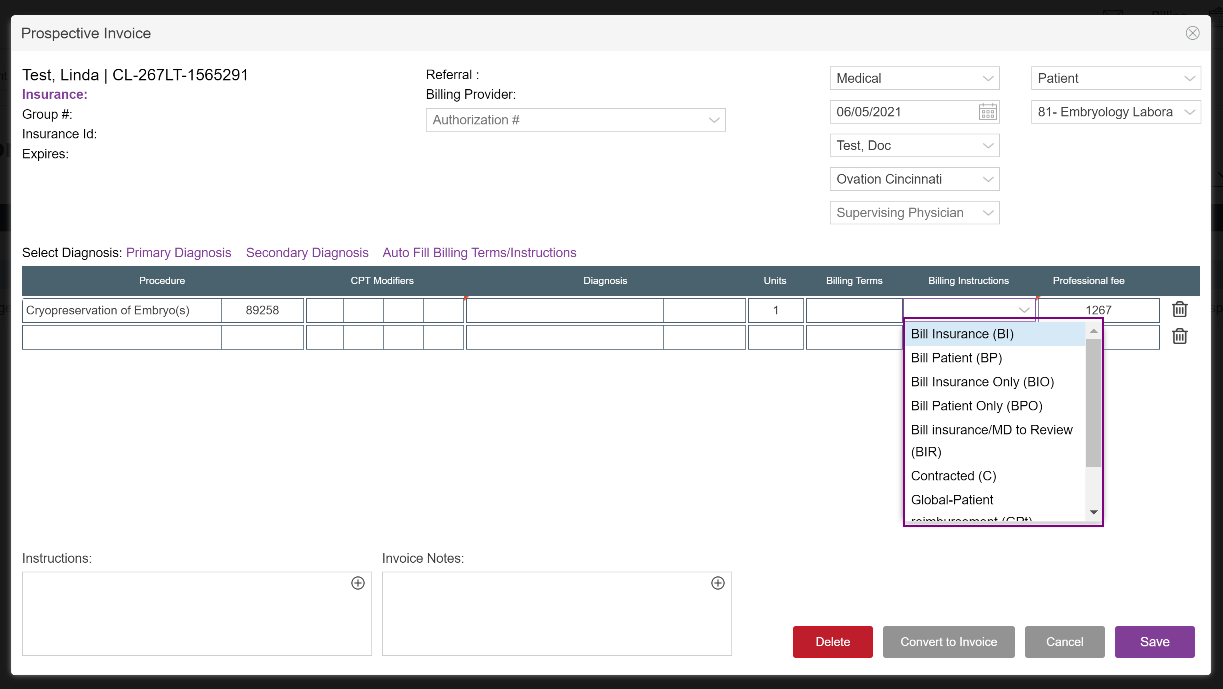
This field directs the office staff regarding the party (patient vs. insurance) that is responsible for the charge and provides instruction as to how the billing should be handled.
In conjunction with billing terms selected (see above):
• BI: bill insurance
• BP: bill patient
• BIO: bill insurance only - this is used when you wish to write off copays or any other portion of the charge that is not covered by insurance.
• BPO: bill patient only - do not submit a charge to insurance.
• BIR: "bill insurance and I will review" - instructs the billing office to bill the patient's insurance and review the EOB with the physician for disposition of any residual balance. This may be used if the physician wants the option of writing off a portion of a charge after it has been paid by the insurer.
• C: contracted insurance - used for patients that have contracted insurance. Instructs the system to bill for copays only for that service on the encounter date.
In conjunction with Package Service Plan (Pkg) billing terms:
Patients that have prepaid for a global service may be billed with one of two options:
• GPt: "Global, bill for patient recovery" - instructs the office to create an invoice for the patient to submit to their carrier for reimbursement.
• GPR: "Global, bill for practice recovery" - in some instances the patient's insurance will have reimbursed the patient with funds that equal her cash global payment to the practice. GPR instructs the billing department to bill the patient's insurance for practice recovery.
Once you have filled in your first line item with the Billing Term and Billing Instructions click on the AutoFill Billing Terms/Instructions for the system to fill in the rest of the line items. You are able to override them if necessary.
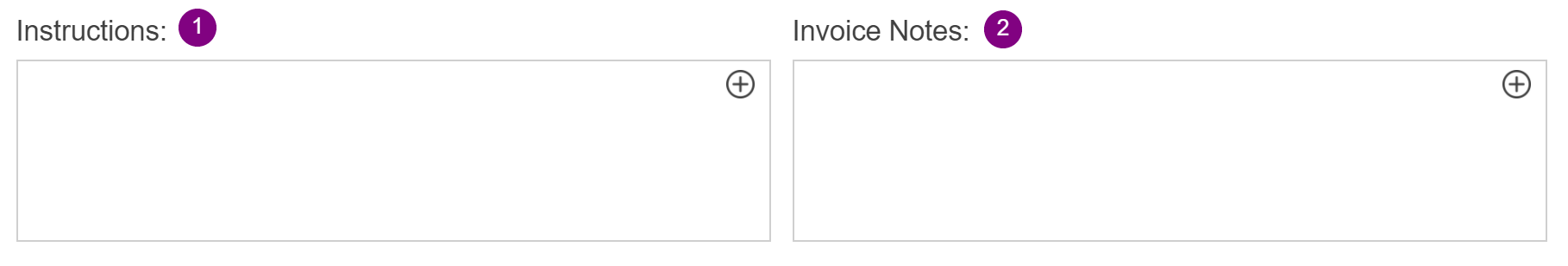
Instructions and Invoice Notes
- If you wish to leave any visit-specific instructions for the billing team, please enter them here.
- You may enter claim notes here; these notes will also carry over and stay with the invoice post-creation.
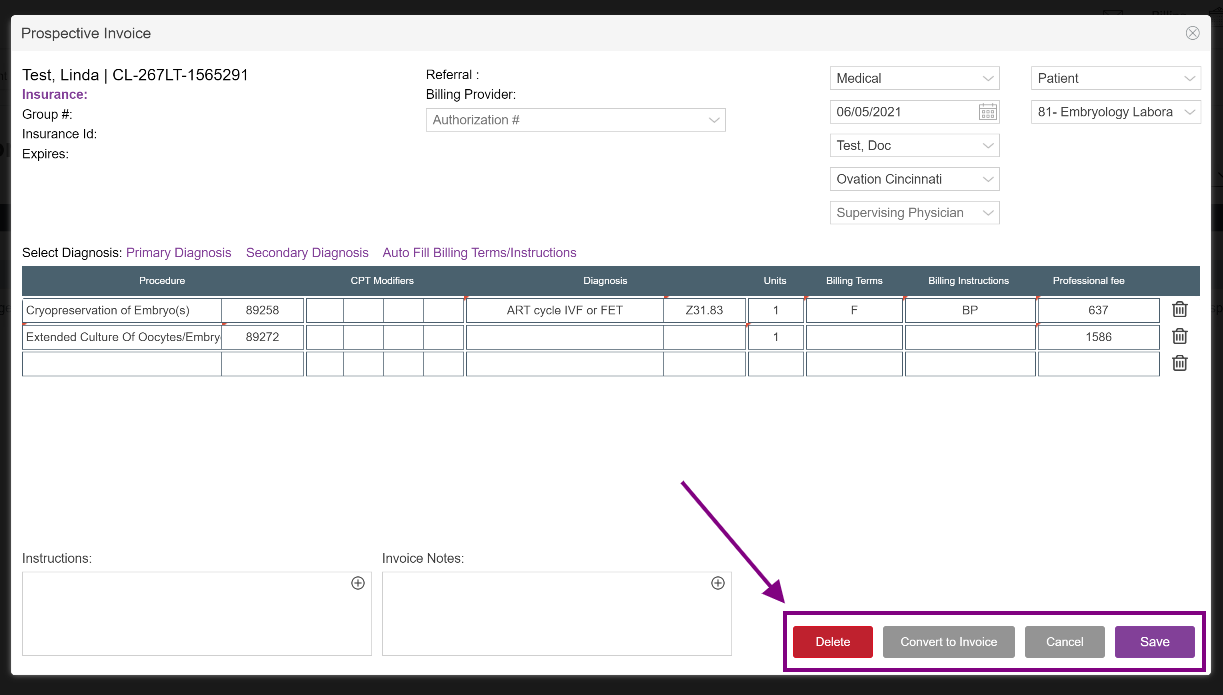
Converting, Saving, or Deleting
Once you are done editing the Prospective Invoice, you can select Convert to Invoice or Save. Examples of all are shown below:
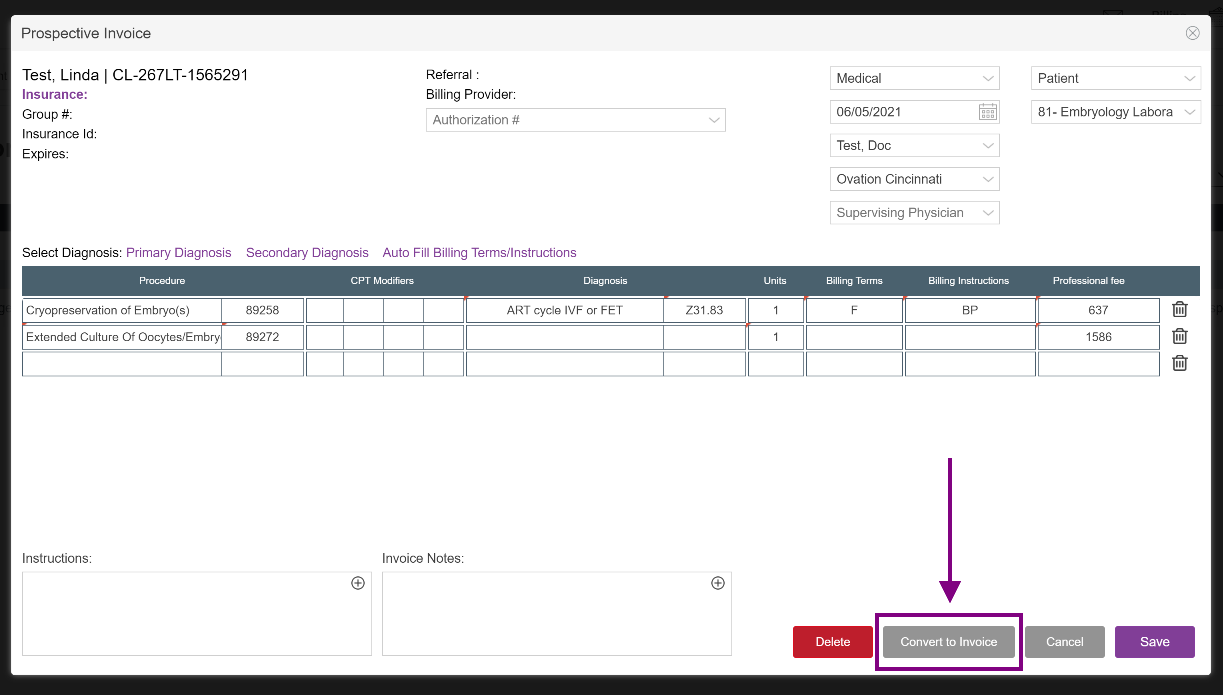
Converting to Invoice
To convert the invoice, click Convert to Invoice.

The Prospective invoice has now been converted to an actual invoice in the patient's accounting section of their record.
All converted prospective invoices will show the gray Converted status in place of the edit option.
Updating and Saving a Prospective Invoice (not converting to an invoice)
You may choose to Save the changes you've made to the prospective invoice rather than convert to an invoice. This may be done for example, if you are working the prospective invoice but want to come back to it later to add information and do not wish to create the invoice yet.

Deleting a Prospective Invoice
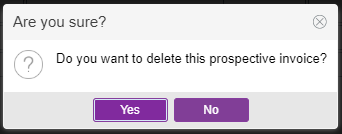
You may delete a prospective invoice in the event that duplicate charges are created.
A warning will pop up to confirm that you are sure that you want to delete this invoice as you will not be able to reverse this action. Select Yes to continue.
**All manuals are compliant with HIPAA regulations. No patient information has been released. All screenshots above were taken from a test clinic with fake patient information.


Heather Yatsko
Comments